
Niger J Paed 2016; 43 (1): 46 - 50
ORIGINAL
Ahmed PA
Pattern of liver diseases among
Ulonnam CC
children attending the National
Mohammed-Nafiu R
Ballong J
Hospital Abuja, Nigeria
Nwankwo G
DOI:http://dx.doi.org/10.4314/njp.v43i1.9
Accepted: 5th August 2015
Abstract :
Background: Diseases
socioeconomic classes while 23
of
the liver contribute to child-
(54.8%) had various forms malnu-
Ahmed PA (
)
hood morbidities and mortality.
trition. Common symptoms in-
Ulonnam CC, Mohammed-Nafiu R
Early recognition and proper man-
cluded jaundice (30; 71.4%), ab-
Ballong J, Nwankwo G
Department of Paediatrics,
agement of liver diseases can
dominal pain (17; 40.5%), fever
National Hospital Abuja
limit the progression to irrepara-
(15; 35.7%), abdominal swelling
Email: ahmedpatience@yahoo.com
ble damage which requires liver
(12; 28.6%) and bleeding (8;
transplant. However, there is scar-
19.0%). The signs included jaun-
city of data in the pattern of liver
dice (30; 71.4%), hepatomegaly
disease in Nigerian children.
(16; 38.1%) and splenomegaly (8;
Objective: To
describe the
pattern
19.0%). Twenty-four (57.1%) had
of
paediatric liver diseases among
chronic viral infections while the
children seen at the National Hos-
others included neonatal hepatitis
pital, Abuja.
syndrome and biliary atresia (6;
Methods: A
retrospective, de-
14.3%), acute hepatitis (6; 14.3%)
scriptive study conducted at the
and chronic hepatitis of unidenti-
Paediatric
Gastroenterology,
fied aetiology (4; 9.5%). Overall,
Hepatology
and
Nutrition
the mean values of the liver en-
(PGHAN) clinic and the Emer-
zymes and serum bilirubin were
gency Paediatric Unit (EPU) of
elevated while the mean values of
National Hospital Abuja, over a 5-
total serum proteins and albumin
year period (2009 – 2014). The
levels were reduced. Five (11.9%)
diagnosis of liver diseases was
children improved and were dis-
made from clinical and laboratory
charged, 15 (35.7%) were lost to
features. The data extracted from
follow up with three deaths.
the retrieved hospital records were
Conclusion: Risk
factors associ-
analyzed.
ated with liver diseases in this
Results: Forty-two
out of
52
study included age over 5 years
documented cases were analyzed.
and lower socio-economic classes.
The children were aged 2 months
Jaundice was the commonest clini-
to
15 years with the mean of 7.24
cal presentation while the most
±
4.77 years. Twenty-six (62.0%)
common aetiology was chronic
were aged >5 years (p>0.05).
Hepatitis B virus infection.
They comprised 31 (73.8%) males
and11
(26.2%)
females;
28
Key words: Children,
Liver
(66.7%) belonged to the lower
Diseases, Pattern
Introduction
viduals, with some age specific features and patterns
which differ from one region of the world to another.
1
Diseases of the liver may be infective, metabolic, toxic,
The clinical features of liver dysfunction may include
autoimmune, vascular or infiltrative in nature. With the
symptoms related to digestion problems such as abnor-
long list of the various aetiologies of paediatric liver
mal fat absorption and metabolism, coagulopathies,
diseases, about ten diseases constitute approximately
blood sugar abnormalities and immune disorders. Others
95% of all cases of cholestasis, and of these, biliary
include features of cholestasis, portal hypertension and
atresia and neonatal hepatitis are responsible for more
eosophageal varices.
than
60%. Diseases of the liver contribute significantly
1
to
childhood morbidity and mortality.
2,
3
The
clinical
Biliary atresia is a liver disease of the newborn which is
presentation of liver diseases vary greatly between indi-
characterized by abnormalities of the intra- and extra-

47
hepatic bile ducts, with incidence rates reported to vary
Methods
between 1 in 8, 000 and 1 in 21, 000 live births. Biliary
4
atresia is a major indication for liver transplantation
This was a retrospective, descriptive study of children
among children.
4
The autosomal recessive disorder,
managed over a five-year period (January 2009 to Janu-
Alpha-1-antitrypsin deficiency, affects 1 in 1, 800 live
ary 2014) at the Paediatric Gastroenterology, Hepatol-
births and is the most common genetic cause of liver
ogy and Nutrition (PGHAN) clinic and the Emergency
disease in children. Viral hepatitis occurs in patients of
1
Paediatric Unit (EPU) of the National Hospital Abuja.
all ages, with about 500, 000, 000 people chronically
The PGHAN clinic runs every Wednesday as a special-
infected with Hepatitis B virus (HBV) or Hepatitis C
ist out-patient referral clinic while the EPU provides 24
virus (HCV) worldwide. Hepatitis B virus (HBV) infec-
5
hours emergency services for all sick children. From the
tion causes both acute and chronic hepatitis which may
EPU, children with liver diseases are referred to the spe-
progress to liver cirrhosis and hepatocellular carcinoma.
cialist clinic for follow-up care.
The diagnosis of HBV rests on the demonstration of
Hepatitis B surface antigen (HBsAg) or anti-HBV core
The hospital records of the children with liver diseases
(anti-HB c ) IgM antibody.
Chronic HBV infection is as-
were retrieved from the Medical Information Depart-
sociated with the persistence of HBsAg and HBV DNA.
ment following due permission. The diagnosis of liver
The Hepatitis C virus (HCV) causes acute hepatitis,
diseases was based on the constellation of clinical and
which also progresses to chronic disease in more than
laboratory features. The data obtained included symp-
70% of affected individuals. Although end-stage liver
toms
and signs suggestive of liver diseases such as fe-
disease can occur in up to 10% of cases, fulminant hepa-
ver, jaundice, abdominal pain, swellings, itching, pale
titis has been described, though it is rare. The diagnosis
stools, bleeding, weakness, vomiting, anorexia, pallor,
of
HCV is suggested by the presence of anti-HCV anti-
hepatomegaly, splenomegaly and ascites. The results of
bodies and confirmed by polymerase chain reaction for
liver function tests such as serum levels of alanine ami-
HCV RNA. Hepatitis D virus (HDV) infection occurs
notransferase (ALT), aspartate aminotransferase (AST),
only in patients who have HBV infection. HDV is pri-
Alkaline phosphatase (AP), prothrombin time (PT) and
marily associated with intravenous drug abuse and it
partial thromboplastin time (PTT), international nor-
usually aggravates on-going liver disease in children
malization ration (INR), serum protein and albumin
with HBV infection. In addition, Hepatitis E virus
were also recorded. The results of viral serology markers
(HEV) occurs in epidemics in parts of the world that
such as HBsAg, HbeAg, and HBV-DNA for hepatitis B
have poor sanitary conditions. Disorders of fat metabo-
infection; HCV, anti-HCV and HCV- RNA for hepatitis
lism usually present in late infancy and early childhood
C
infection as well as HIV screening were also captured.
while neoplastic diseases of the liver among children
Other investigation reports reviewed were liver biopsies,
and adolescents differ from the types observed among
abdominal ultrasonograpy and abdominal computed
adults.
tomography (CT) or magnetic resonance imaging (MRI)
reports. Four patients had liver biopsies done, while ge-
Chronic hepatitis is traditionally defined as an inflam-
netic information and enzymatic assay could not be done
matory condition of the liver characterized by the persis-
due lack of facilities.
tence of biochemical and histologic abnormalities for
more than six months. However, irreversible changes
The children were classified into three broad categories;
may occur in children within those six months. These
namely, infective, non- infective (metabolic, congenital,
chronic hepatitis conditions may be viral infections,
cholestatic, neoplastic) and idiopathic liver diseases.
autoimmune processes, and exposure to hepatotoxic
Specific diagnoses were categorized as chronic liver
drugs as well as cardiac, metabolic, or systemic disor-
disease (CLD) when symptoms persisted beyond six
ders. Most cases of acute hepatitis in children resolve
months of follow-up care, with or without identifiable
within three months. Progressive liver dysfunction af-
viral serological markers. The group classified as idio-
fects childhood nutrition and may be complicated by
pathic had no identifiable cause while acute hepatitis
growth retardation. Unfortunately, the timely recogni-
had symptoms with resolution within less than six
tion of severe liver disease in children remains a major
months and were negative for serological markers. A
challenge. One factor contributing to this challenge is
few patients were screened for cytomegalo-virus (CMV)
the manifestation of injuries to the paediatric liver in a
and toxoplasmosis. Facilities for other serological mark-
finite number of ways, hence different hepatic disorders
ers were not available. Demographic characteristics and
often have virtually identical initial presentations. Early
outcome of the care for the children were obtained and
intervention may reduce the progression of liver diseases
classified. Data were analyzed using SPSS 20 version.
from initial inflammation to scarring with irreparable
Pearson Chi-squared test was used for the comparison of
damage in the form of cirrhosis and/or cancerous trans-
categorical data and p values <0.05 were considered
formation.
1,
4, 6
Therefore, the aim of this review was to
statistically significant.
determine the pattern of liver diseases among children at
the National Hospital, Abuja.
Results
A
total of 52 cases were documented in the records from
the clinic and the EPU, out of which 42 cases were ana-

48
lyzed. The age of the children ranged from 2 months to
Table 4: Diagnoses
among children
with liver
diseases
15years with the mean (± SD) of 7.24 (± 4.77) years.
Diagnoses
Number (%)
There were 31 (73.8%) males and 11(26.2%) females
CLD
(viral hepatitis)
24
(57.1)
with a male-to-female ratio of 2.8:1. Sixteen (38.0%)
Acute
hepatitis
6
(14.3)
subjects were aged 5 years and below; half of these were
CLD
(unknown cause)
4
(9.5)
aged
less than one year. The remaining 26 (62.0%) sub-
Neonatal hepatitis syndrome (NHS)
3
(7.1)
jects were older than five years. The differences in the
Biliary atresia
3
(7.1)
proportion of children in the comparison age groups
Fulminant hepatitis
2
(4.8)
were not significant (p = 0.897) (Table 1). The distribu-
Cholestatic hepatitis(ciliopathy/ choledochal cyst)
2
(4.8)
Portal hypertension with oesophageal varices
2
(4.8)
tion according to the socioeconomic classes were as
Malignancy (hepatoblastoma)
1
(2.4)
follows; 28 (66.7%) in the lower socioeconomic class, 6
Galactosaemia
1
(2.4)
(14.3%) and 8(19.0%) in the upper and middle socioeco-
Some children had more than one diagnostic classification; CLD –
nomic
classes respectively. Nineteen (45.2%) of the
chronic liver disease
subjects were fully vaccinated for HBV during infancy;
19
(45.5%) had normal nutritional status while 23
CLD of viral aetiology formed 57.1% of all the children
(54.8% had various forms malnutrition with no statisti-
studied. Non- infective cases, namely, biliary atresia,
cally significant difference in the proportions (p =
cholestatic hepatitis, hepatoblastoma and galactosaemia
0.058) (Table 2).
accounted for 21.4% s while idiopathic cases included
acute hepatitis 14.3%, CLD 9.5% and NHS 7.1% as
Table 1: Age
and sex
distribution of
children with
liver
shown in Table 4. Of the 24 (57.1%) subjects positive
diseases
with viral serological antigen markers, 18 (75.0%) were
Age
groups
Males
Females
Total (%)
positive for Hepatitis B surface antigen (HbsAg); 10
(years)
with HbeAg and 6 with elevated HBV DNA viral load.
0-5
12
4
16(38.0)
Χ2
= 0.217
Five (11.9%) children were positive for hepatitis C anti-
>5-10
10
3
13(31.0)
gen and anti- HCV antibodies, some with co-infections
>10- 15
9
4
13(31.0)
p =
0.897
(Table 5).
Total
31
11
42(100.0)
Table 5: Distribution
of Infective
children with
liver diseases
Table 2: Distribution
of children
with liver
diseases according
to
age and nutritional status
Infective category
Number (%)
Age
groups
Normal
Under-
Over-
Total
HBV( 10 HbeAg pos; 8HbsAg carriers)
18
(42.9)
(years)
nutrition
weight
HBV-HCV co-infection
1
(2.4)
Χ
=9.125
2
0-5
4
9
2
16
HCV
(HCV antibodies)
2
(4.8)
>5-10
7
2
5
13
p
=
HCV-HIV co-infection
1
(2.4)
>10- 15
8
3
2
13
0.058
HCV-CMV co-infection
1
(2.4)
Total
19
14(33.3)
9(21.4)
42
CMV-Toxoplasmosis co-infection
1
(2.4)
(45.2)
(100.0)
The mean (±SD) values of liver enzymes and serum
Figures in parentheses represent percentages of the total in the row
bilirubin were elevated, with low total serum proteins
and albumin levels (Table 6). Twelve (28.6%) subjects
The most common symptoms included jaundice (30;
received treatment with antiviral agents and interferon; 5
71.4%), abdominal pain (17; 40.5%), fever (15; 35.7%),
(41.7%) of these 12 children improved with sero-
abdominal swelling (12; 28.6%) and bleeding
conversion and were discharged. One subject with bil-
(8; 19.0%). Physical findings included hepatomegaly
iary atresia had liver transplant overseas, while 15
(16; 38.1%), pallor (14; 33.3%) and splenomegaly
(35.7%) were lost to follow up (Figure1). There were
(8; 19.0%) as shown in Table 3.
three deaths, two of which had unknown aetiology and
presented with encephalopathy
Table 3: Frequencies
of symptoms
and signs
of liver
diseases among
children
Table 6: Liver
Functions profile
of children
with liver
diseases
Features
Frequencies
Percentages
Parameters
Mean
Std. Deviation
Symptoms
values
Jaundice
30
71.4
Serum Aspartate aminotransferase (AST)IU/L 135.23
171.81
Abdominal pain
17
40.5
Serum Alanine aminotransferase (ALT)IU/L
176.80
376.40
Fever
15
35.7
Serum Alkaline phosphatase (AP)IU/L
261.23
196.22
Abdominal swelling
12
28.6
Serum Gamma glutamyl transpeptidase (GGT)
Vomiting
8
19.0
IU/L
155.73
259.66
Weakness
8
19.0
Conjugated serum bilirubin (umol/L)
22.15
65.37
Bleeding
8
19.0
Total serum bilirubin (umol/L)
79.05
126.21
Pale stool
7
16.7
Total serum proteins (g/L)
33.86
35.28
Anorexia
7
16.7
Serum albumin (g/L)
16.70
17.85
Itching
4
9.5
Unconsciousness/restless
2
4.8
Signs
Hepatomegaly
16
38.1
Pallor
14
33.3
Splenomegaly
8
19.0
Ascites
5
11.9
Coma
2
4.8
49
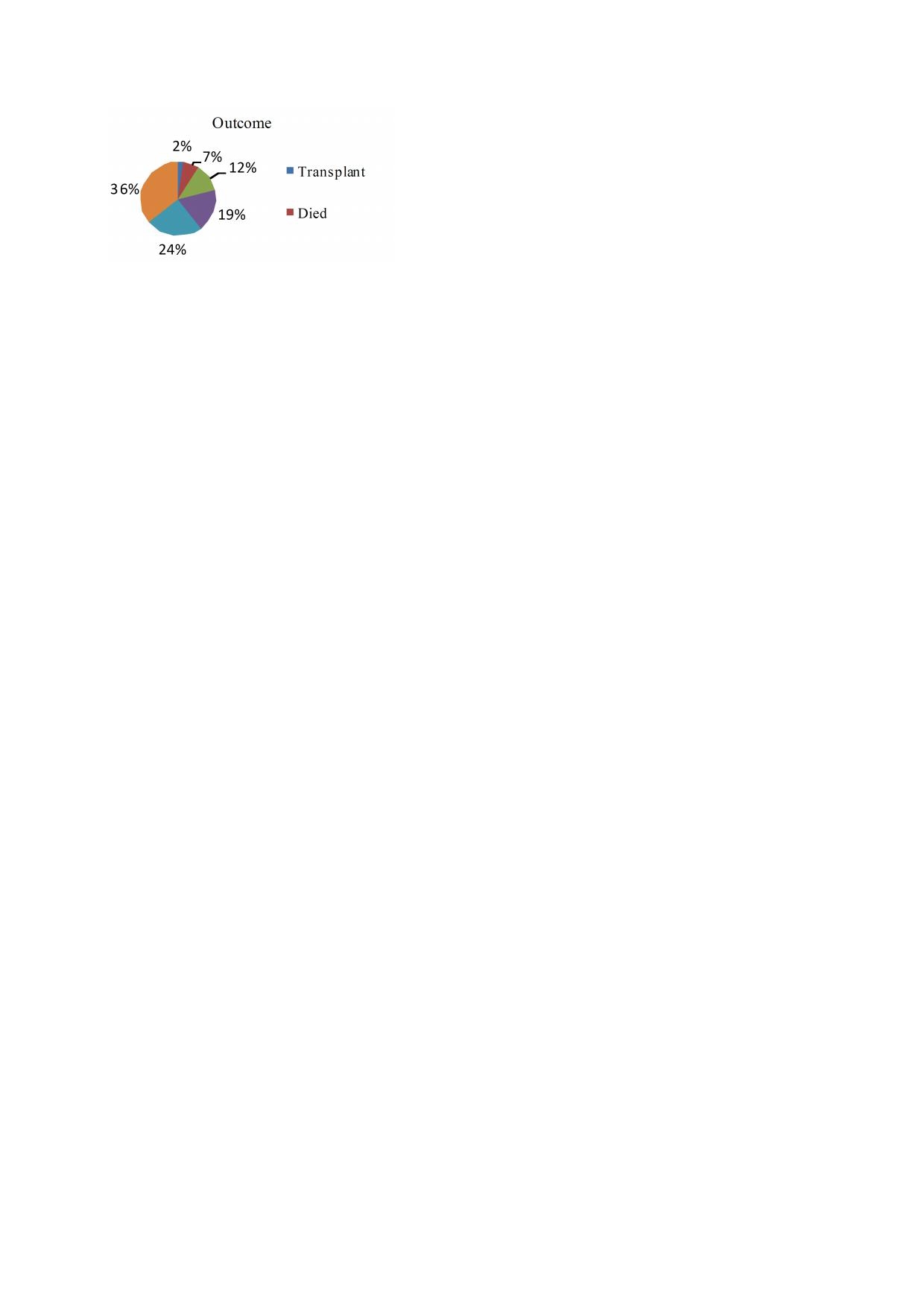
Fig 1: Outcome
of children
with liver
diseases
and bleeding. In a report by Dar
et al
10
on
186 children
Outcome
less
than 18 years, jaundice was reported among all the
2%
children presenting with acute hepatitis, and 75 percent
7%
of
those presenting with chronic liver diseases. Some
12%
Transplant
children in this report, presented with features of portal
36%
hypertension and esophageal varices such as hepa-
19%
Died
tosplenomegaly, ascites, gastro-intestinal bleeding and
encephalopathy. These features were suggestive of fairly
24%
advanced liver diseases with decompensation present at
presentation. Such children were classified under grades
B
and C of the Child- Pugh scores. The children had
deranged values of laboratory parameters; specifically
Discussion
elevated liver enzymes levels and bilirubin levels and
low
albumin levels. These findings suggested both acute
This
hospital-based descriptive review focused on the
and
chronic liver pathology. According to the Child-
Pugh
scoring system, total serum bilirubin greater than
10
spectrum
and
magnitude
of
liver
disorders
among children aged less than 16 years who were man-
50µmol/l, serum albumin less than 2.8g/dl, prolonged
aged over a five-year period in a tertiary health centre.
prothrombin time and INR level greater than 2.3, moder-
The demographic characteristics suggested that males
ately severe ascites and hepatic encephalopathy pre-
and
children from lower socioeconomic classes were
dicted mortality. Some of the children in this report had
more
frequently affected by liver diseases.
3,
7- 9
The
age
chronic liver disease that met the above-stated criteria,
of
the children in this study ranged between 2 months
though endoscopy was not available for the children
and
15 years with the mean of 7.24 ± 4.77 years. This
with
bleeding varices.
was
similar to the findings reported by Dar
et al ,
10
who
reported the mean age of 9.34 ± 4.8 years (range of 1-18
The most common aetiologic group in the present study
years). The age data in the present study were higher
was
infective (viral) hepatitis, especially Hepatitis B
than
the mean age of 4.8 ± 0.3 years (range 5 months
infections. This report was similar to the findings in a
and
14 years) reported by Alam et al . Children aged
9
retrospective analysis of 300 children with various liver
over five years accounted for 62 percent of the study
diseases, at two major teaching hospitals of Karachi
population in the present report. This observation may
where acute viral hepatitis and its sequelae were the
most frequent (31 percent) of all hepatic ailments. The
8
suggest exposure to preventable liver infections early in
life in this population. Various forms of malnutrition
5
World Health Organization (WHO) reported that about
(underweight, marasmus and overweight) were observed
two billion people are infected with the Hepatitis B virus
among 54.8 percent of the children studied while 21.4
(HBV). In highly endemic areas, HBV infections in chil-
percent was overweight. Under- nutrition may be a di-
dren are most commonly spread from mother to child at
rect consequence of liver diseases while overweight and
birth or from person to person in early childhood and
adolescence. Children aged above five years accounted
5
obesity are predisposing conditions. In a retrospective
study of 79 children with chronic liver diseases whose
for
66.7 percent of all the known infective cases in this
mean
age was five years, reported by Al-Lawati
et al ,
11
study. Reports have shown that the persistence of viral
growth retardation was recorded among 75 percent of’
infections
in the liver predisposes to cirrhosis and hepa-
the
children.
tocellular carcinoma. The diagnosis of HBV was based
on
sero-positivity for HbsAg and HbeAg as well as the
The recent rise in the prevalence rates of obesity and
HBV DNA viral load in a few cases who could afford
overweight in the United States has resulted in the emer-
the test where it is available. Children with detectable
gence of non- alcoholic fatty liver disease (NAFLD) as
HBsAg for a period up to six months with or without
the leading cause of chronic liver disease among chil-
concurrent HBeAg were considered to have chronic
dren and adolescents in the United States.
12
In
addition,
HBV infection. The presence of HBeAg only indicates
emerging data suggest that children with non-alcoholic
that the child is highly infectious. Other makers of infec-
steatohepatitis (NASH) progress to cirrhosis which may
tion such as the assay of immunoglobulins to hepatitis
ultimately increase liver-related mortality.
12
However,
core antigen (IgMHBcAg) and the newer HBsAg quan-
due to non-availability of advanced biochemical labora-
tification assay are not yet routinely evaluated due to
tory and limited facilities for biopsies, the inability to
non-availability and high cost. Hepatitis C infection
search for some of these metabolic disorders in the pre-
cases were also recorded in this study, though less com-
mon than expected.
13
sent report may be a limitation in this study. Liver his-
Most often, HCV infection is ac-
tology remains the gold standard for assessing hepatic
quired at birth in the younger child but adolescents can
steatosis. Nevertheless, only four (9.5 percent) children
also acquire the infection through activities which facili-
in
our series had liver biopsy. This rate was lower than
tate blood contacts such as intra venous drug use, shar-
ing
needles and high-risk sexual behaviors.
14
the 30/164 (18.3 percent) reported in the Dhaka Shishu
The
odds
Hospital study.
9
of
a child acquiring HCV from an infected mother is
Jaundice was the most common clinical feature in over
1:20.
14
Reports show that spontaneous clearance of
70
percent of the children in this study. Others included
HCV infection can occur in about 40 percent of new-
abdominal pain and swelling, fever, vomiting, weakness
borns who acquired the disease vertically, by the age of
50
two
years, and sometimes up to 7 years. Co-infections
14
tem human disorders caused by a multitude of largely
were recorded in the present study, with HBV/HCV co-
unrelated genes that affect ciliary structure/function. The
infection and HBV/HIV co-infection. HBV/HCV co-
mode of inheritance is recessive, either autosomal or X-
infected persons have been shown to have more severe
linked, with strong evidence of genetic modifiers which
determine expressivity.
16
liver injuries and higher chances of progression to cir-
rhosis or cancerous transformation. CMV co-infections
15
with HCV and toxoplasmosis were also identified in this
Some children had liver diseases of unknown aetiology,
report. This observation underlines the importance of
most of whom had complete resolution and were dis-
charged home. Dar et
al reported 52 percent with no
10
testing for other non-hepatitis virus in any suspected
case of liver disease.
aetiology (cryptogenic) in a hospital- based descriptive
study. Some of the reasons limiting diagnosis of specific
Neonatal hepatitis syndrome and biliary atresia ac-
liver patterns included the non-availability of routine
counted for 14.2 percent of liver diseases among infants
biopsies, specific diagnostic tools for HbsAg quantifica-
in
this study. Biliary atresia presenting as cholestatic
tion levels, routine HBV- DNA (viral load) and mag-
liver disease, may be caused by intra-or/and extra-
netic resonance elastography (MRE) which accurately
hepatic bile ducts obstruction. It is the major indication
detects fibrosis. About a third of the children in the pre-
for liver transplantation in children. Early presentation
4
sent
study were lost to follow up for various reasons
is
most desirable and portoenterostomy surgery (Kasai
such
as poor finances and non-availability of immediate
procedure) is best carried out within 100 days of life.
cure.
The
success of this procedure in the establishment of
bile
drainage, is variable and up to 40 percent of chil-
dren
may develop significant fibrosis and progress to
Limitation
require liver transplantation within the first few years of
life. One of the children in the present study had liver
4
Incompleteness and loss of data were noted in the pre-
transplant within the first two years of life. Other rare
sent
study. Other limitations included lack of adequate
causes of liver disease, such as ciliopathy, hepatoblas-
investigative capacity mostly due to non-availability of
toma
and galactosaemia were seen in this report. A case
advanced biochemical laboratory and financial con-
of
liver ciliopathy presented acutely with massive GI
straints.
bleeding, hepatomegaly and ascites with deranged liver
functions. The diagnosis was made with liver biopsy.
Conflict of interest: None
Ciliopathies are an emerging class of genetic multisys-
Funding: None
References
1.
D’Agata ID, Balistreri WF.
7.
Burki MK, Orakzai SA. The
13.
Mack CM, Gonzalez-Peralta RP,
Evaluation of liver disease in the
prevalence and pattern of liver
Gupta N, Leung D, Narkewicz
paediatric patient. Paediatrics in
disease in infants and children in
MR,
Roberts EA, Rosenthal P,
Review 1999; 20 (11): 376 -390.
Hazara Division .
J Ayub
Med
Schwarz KB. NASPGHAN prac-
2.
Okonkwo U, Nwosu M, Boju-
Coll Abbottabad 2001; 13(1): 26-
tice guidelines: diagnosis and
woye B. The predictive values of
28.
management of hepatitis C infec-
the
Meld and Child-Pugh scores
8.
Mehnaz A, Billo GA, Zuberi SJ.
tion in infants, children and ado-
in
determining mortality from
Liver disorders in children. J Pak
lescents. J
Pediatr Gastroenterol
chronic liver disease patients in
Med Assoc 1990; 40: 62- 64.
Nutr 2012; 54:838-55.
Anambra state, Nigeria. Internet
9.
Alam MJ, Ahmed F, Mobarak
14.
Narkewitz MR. Hepatitis C in
J Gastroenterology 2010; 10 (2).
R,
Arefin S, Tayab A, Tahera A,
children. American liver founda-
3.
Sabir OM, Ali AB, Algemaabi O.
Mahmud S. Pattern of liver dis-
tion online article. Link:http://
Pattern of liver diseases in Suda-
eases in children admitted in
www.liverfoundation.org/
nese children. Sudan
J. Med
Sci
Dhaka Shishu Hospital. Int
J
chapters/rockymountain/
2010; 5(4): 285-288.
Hepatol 2010; 1(3):18-24
doctorsnotes/paediatrichcv/. Ac-
4.
Petersen C. Pathogenesis and
10.
Dar
GA, Zarger SA, Jan K,
cessed on 11/11/2014.
treatment opportunities for bil-
Malik MI, Mir TA, Dar MA.
15.
Chu
CJ, Lee SD. Hepatitis B
iary atresia. Clin
Liver Dis.
2006;
Spectrum of Liver Diseases
Virus/Hepatitis C Virus Co-
10:73 – 88.
among Children in Kashmir Val-
infection: Epidemiology, Clinical
5.
World Health Organization.
ley. Academic
Med J.
India 2014;
Features, Viral Interactions and
Prevention & Control of Viral
2(3):80 – 6.
Treatment. J
Gastroenterol Hepa-
Hepatitis Infection: Framework
tol. 2008; 23(4):512-520 .
for
Global Action. WHO 2012;
Eun
Lee J, Gleeson JG Review:
.
11.
Al-Lawati TT;George M;Al-
16.
hepatitis@who.int.WHO.int/
Lawati FA. Pattern of liver dis-
A
systems-biology approach to
topics/hepatitis
eases in Oman. Ann
Trop Paedi-
understanding the ciliopathy dis-
6.
Akinbami FO, Venugopalan P,
atr 2009; 29(3):183-9.
orders. Genome
Medicine 2011,
Nirmala V, Suresh J, Abiodun P.
12.
Loomba R, Sirlin CB, Schwim-
3:59.
Pattern of chronic liver disease in
mer
JB, Lavine JE. Advances in
Omani children- A clinicopa-
Paediatric Nonalcoholic Fatty
thological review. West
Afr J
Liver Disease. Hepatol
2009; 50
Med 2004; 23(2):162-166 .
(4):1282-1293.